The F-word
- Megan Jacklin

- Apr 27, 2017
- 5 min read
This week was a big week: my official OB appointment with Dr. Farringer. Jillian was able to come and meet him and see where I will be spending the next 29 weeks. Baby Girl looked beautiful and was measuring well (3 days over gestational age – maybe I should lay off the sweets a little?).
One small caveat -- my prenatal screening panel was done at CCRM back in October. Dr. Farringer looked over the results and debated whether or not I should have them redone.
During the appointment we finalized the "birth plan" - which is going to be a scheduled repeat c-section.
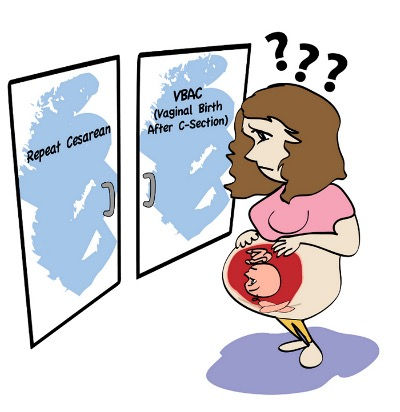
"Did we have a discussion about attempting a TOLAC?" (trial of labor after cesarean)
"Yes. You told me I wasn't your favorite candidate."
"And did that satisfy you?"
"Yes." I giggled again "I already had my trial of labor and it was a huge failure."
For those of you unfamiliar with how Jacob came into this world. My water broke when I was 3 days past my due date. Since I was GBS negative I could labor at home until contractions were regularly unbearable. I did all of the at-home support I could: walking, birth ball, I even went and got a massage. 9 hours later I went into the hospital - vomiting from the pain. I was a whopping 2 cm dilated. This is about the diameter of a sliced grape. Usually we don't admit patients that are less than 4 cm -- but because I was an employee-- and clearly miserable - I bought myself what we call a "Pity Admit." Right at shift change - yes - I was that patient.
Admission labs were drawn and I immediately caved and got an epidural within 45 minutes. I had gotten to 3cm when my charge nurse came in to tell me some ominous news: "Your white count is 22." (double what it should be normally -- indicating that my body was working hard to fight off an infection.)
She met my eyes and I could see the hope fade out of them -- reflecting my own.
"We are going to start you on triples (three different kinds of antibiotics) - and watch you throughout the night." This is nurse-speak for "please don't have your body (or baby) misbehave for the rest of the shift."
She knew that I had been hit with the curse of the nurse.
I knew I was doomed. My early rupture - my stupid thick uncooperative cervix - my sick and tired body. It was all a bad omen. But I gave myself a "trial of labor." I spent the night getting turned every hour - antibiotics hung every two. I had reached 4cm (which is about the diameter of a sliced banana) at a little after midnight. I turned the fetal monitor as far away from me as possible. I didn't want to read my strip - I just wanted to sleep and I willed my body to respond to the maximum dose of Pitocin coursing through my veins. At 5:30 in the morning - just when dawn was creeping in-- the doc entered my room and checked me. "Hon, you're still at 4." I nodded knowing what this meant-- trying holding back tears -- not wanting to look pathetic and weak. "Technically I can give you another 6 hours and check again. Baby looks good... but I'm worried about how much longer I want to press that luck. It's entirely up to you, Megan, how you want this to go."
It was an easy call. "I'll do the section. I've got my night shift crew on. I don't want to have to rush back because of Baby looking like crap." (It's funny how even talking about Jacob - I referred to him as the general "Baby" as if I was talking about a patient I had been monitoring). My message was understood: I would rather go back in a nice controlled trip to the OR instead of a crash scenario. She patted me gently on the leg -- "We will get things going then."
As she left I burst into tears. I had failed. My body was pushed to the limit and I couldn't do what I've helped countless women do over the last several years. Officially it would go down in my medical record as "primary cesarean section for failure to progress." Failure to progress. Failure. That is a permanent mark on my medical history. It's a stigma that overshadows the entire obstetric community. Even as a nurse taking care of your laboring patient -- you NEVER want to have to take her back to the OR. Because it feels like you have failed her too.
It falls just below the other F-word you don't want to have to go back to the OR for: Fetal intolerance to labor. Which is exactly what I wanted to avoid.
I pulled myself together and I realized that it was now an hour before shift change and I was making my co-workers do a c-section. Damn it! Yet again I was that patient. Twice in one shift! Not to mention that Jacob would be an automatic NICU admission because of the infection. He would need antibiotics and labs as well for at least 48 hours.
Now fast forward 3 years later to Dr. Farringer's office -- facing the options of whether or not to TOLAC.
"I'm fine with a scheduled repeat."
He gave a quick nod -- knowing that he didn't need to say any more.
Here's a secret: before I was even pregnant I had been watching the different docs with their suture techniques in the OR. Dr. Farringer always left the nicest looking incisions. That's what first drew me to him as a potential OB. The second reason is an encounter I had with him as a nurse during a heartbreaking delivery. A patient that wasn't even his own. What I witnessed convinced me that he had a beautiful heart. I want him taking care of me in my time of need. Maybe I'll share that story at a later time -- but for right now -- I'll keep it in the vault.
Baby Stats:
Gestational age: 11 weeks 5 days
Size: Fig
Development: tooth buds, hands opening and closing, diaphragm working (which means hiccups abound!)
Stork Sensations: tired, tired, tired. I haven't fallen asleep at work but I have fallen asleep before 8 pm a few nights this week. Two more weeks until I enter the "Golden Age of Pregnancy"

Bonus fact: Jillian’s birthday was on 4/26 – I am glad that she was able to make it and see this little one first hand. Happy Birthday, Mama!!

Comments